AACtual Therapy: On Motivation and AAC with Samantha Weatherford
Motivating clients to use and learn more about their AAC systems can sometimes be a challenge, particularly if the learner has had decades of life experience before being introduced to AAC. In this post,  we welcome SLP Samantha Weatherford, who works in the areas of early intervention and adult rehabilitation. She blogs at So To Speak regarding the educational, professional, and clinical processes of becoming an SLP. She resides in Delaware with her cat Simon, and took some time to share her thoughts about helping adult clients get motivated to use AAC.
we welcome SLP Samantha Weatherford, who works in the areas of early intervention and adult rehabilitation. She blogs at So To Speak regarding the educational, professional, and clinical processes of becoming an SLP. She resides in Delaware with her cat Simon, and took some time to share her thoughts about helping adult clients get motivated to use AAC.
On Motivation and AAC
Have you ever started the AAC training and trialing process with an adult client and realized, “This person is just not interested in being here or doing this?” Maybe it’s just me, but I feel like this happens quite often. I would never rule-out the possibility for AAC eligibility as a result of an hour long evaluation, but many times I see that caregivers are very gung-ho to get an AAC system put in place, while the client isn’t necessarily on board.
How then, do we get a client motivated? Can you? (Spoiler alert: you can try!)
- Reinforcers – We all know this. I ask the client and caregivers in the evaluation: What do you like to do? Who is important to you? What are a few of your favorite things? Then hopefully, if some of those things are tangible, we can use them to get the person motivated to use their communication aid. This tactic tends to work more for the developmental disability population in regard to requesting, but it can be helpful when an adult with an acquired disability wants to talk about what makes them who they are – and they haven’t been able to in a long time!
Many clients are motivated by music – this switch access iHome by Enabling Devices is often very motivating and reinforcing.
- What is this person’s best sensory input modality? – I’m currently working with several young adults with diagnoses of Deaf/Blindness as well as severe physical disabilities, which can prove to be a bit of a challenge. For one patient who is completely blind, we use tactile input to help him learn more about his choices and how to access them. For example, I’ve Velcro-ed a rough material onto the “stop” button, and a soft material onto the “more” button. I assist him, hand over hand, to initially find the buttons and access the message and immediately reinforce the message. Another patient just responds better to real pictures rather than line drawings – Why? I don’t know! It is just what works and gets them motivated to do more! Explore with your patients, and figure out how you can get information in, so they can get information out!

- Success! – If I went to the gym every day for a year and didn’t feel satisfaction and success with my exercise I probably wouldn’t go anymore. Because it is
 not motivating to fail. When your client does something well, make sure you let them know and encourage them to do it again. I’m working with a young woman right now who is trialing some eye gaze systems. It took us a long time to figure out that this is the best way for her to experience success with communication and until we figured it out she would shut down as soon as she came in the room. Don’t make your therapy sessions painful by trying to force a communication aid that clearly does not interest the person and that they might not be experiencing success with!
not motivating to fail. When your client does something well, make sure you let them know and encourage them to do it again. I’m working with a young woman right now who is trialing some eye gaze systems. It took us a long time to figure out that this is the best way for her to experience success with communication and until we figured it out she would shut down as soon as she came in the room. Don’t make your therapy sessions painful by trying to force a communication aid that clearly does not interest the person and that they might not be experiencing success with! - Heart-to-Heart – This is not something I particularly enjoy doing. I recently saw a patient with a degenerative disorder whose speech is 98% unintelligible to a familiar listener with context. We tried every system I could think of but she just was not motivated to use it in a functional, every day sense. And finally I had to say, “I know you’re trying really hard to make me and your caregivers happy, but YOU want to keep using your speech. I respect that and I understand it, but we’ve got to face the facts here and make a decision.” Long run, she still wanted to use her speech but we had the tough love talk that we needed to have so she could understand where her caregivers were coming from. We can’t keep up therapy forever without progress, even if it is great fun.
- Anticipation – Often you may find that when an adult has a disability their caregivers do a lot for them. Which is fantastic and I love that so many of my clients have such great support systems. However, always anticipating what a person needs is like cutting off a person who stutters. It reduces the opportunity to communicate before the communicating gets to even occur. I see a lot of patients whose caregivers want a communication device but when we probe to see what this person would need to actually communicate…there is not a lot because everything is done for them. We may think of doing this with a child (i.e. putting something they need on a shelf and acting the fool when they point and vocalize to get it) but it is something to consider in the event that you observe a lot of anticipating and routine for an adult. I don’t love this strategy because often caregivers know what a person needs via behavior (“When he rocks that way he’s hungry”) and I don’t want to give the idea that we should not respond to known communicative attempts, so tread lightly here. Robin Parker wrote about more ways to create communication opportunities for adults which can be found HERE!
- He’s just not that into you – Sometimes we have to take a step back and say, “Is it me?” And sometimes…yes, it is you. You are not motivating or maybe even de-motivating (if that’s a word) for the client. That is okay (I know it hurts…we SLPs are a sensitive bunch and we like to be good at everything.) See if your practice wouldn’t mind you switching with a different clinician for a session or coach a motivating caregiver through your session. If you observe no difference in their response when you do this then maybe they just aren’t internally motivated or they’re feeling overwhelmed by something else. If there IS a difference in their response, then honor the client’s preference just like you would for someone who can say, “Hey I don’t like you, I want a different SLP!”
- On that note – Consider your environment. You can easily shut down a whole session with just the way you look. I do not wear scrubs because half of my patients think they’re coming to see the doctor and it stresses them out – why should I propagate the idea by dressing like a medical professional when I don’t
 work in a hospital? Are any of the caregivers overwhelming for this person? I have seen many patients whose caregivers are awesome, but very excited and get a little carried away trying to encourage the patient to use a communication aid. Would this person mind stepping back, or even out for a minute just to see how the patient does without that prompting and cueing? Maybe just try changing rooms – go on a little field trip, or consider doing therapy in their natural environment if possible.
work in a hospital? Are any of the caregivers overwhelming for this person? I have seen many patients whose caregivers are awesome, but very excited and get a little carried away trying to encourage the patient to use a communication aid. Would this person mind stepping back, or even out for a minute just to see how the patient does without that prompting and cueing? Maybe just try changing rooms – go on a little field trip, or consider doing therapy in their natural environment if possible.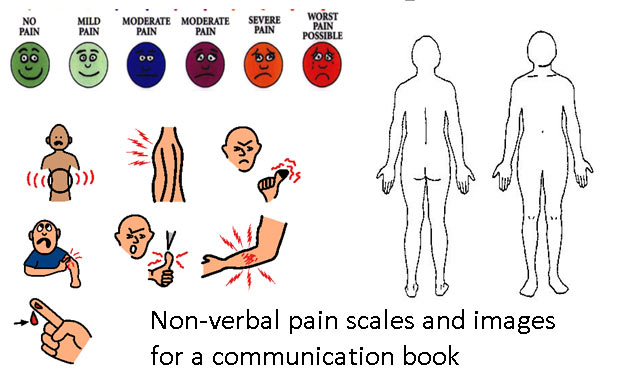
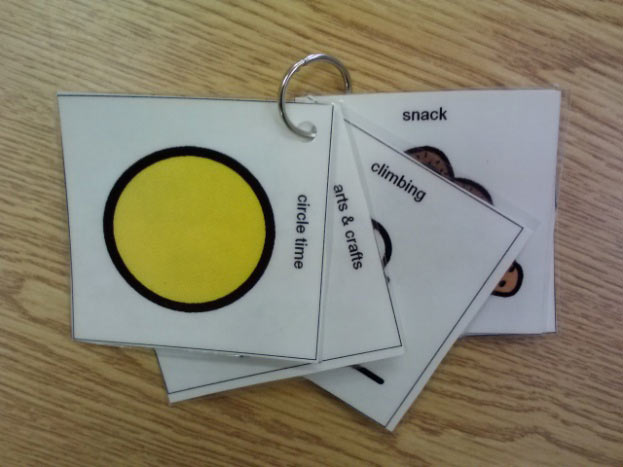
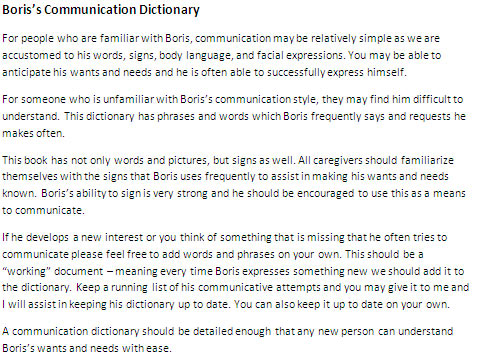
At the end of the day you cannot make anyone use an AAC system and we don’t want to recommend something that is going to end up with dead batteries in a closet somewhere. If you have tried your hardest and put in your best effort and you don’t feel that the client is motivated to use a communication aid then that too, is a recommendation. Typically in this situation I suggest a possible future re-evaluation in the event that the client’s communication needs change. I also try at this point to put something no-tech in place for basic communication and health status (communication book, alphabet board, gesture dictionary, picture ring) because I do not like feeling like I’m leaving a family high-and-dry.
Hopefully though, using some of these strategies or one of your own, you get through and find a communication system that is the best fit for your client. Please share below if you have any tricks of the trade that keep your adult clients motivated and interested!
Filed under: PrAACtical Thinking
Tagged With: AACtual therapy, adults, motivation, Samantha Weatherford
This post was written by Carole Zangari


1 Comment
This is a BIG issue with my students. I work with young adults with developmental disabilities. It is often difficult to move beyond food reinforcement. I have had success using my iPad for choice making and commenting. I have a velcro communication board with screen shots of a few highly stimulating apps. My students often don’t have the motor skills to be able to actually select and open the apps on the iPad. They make a choice by giving me the icon and then I open it for them. I also like to play music and video clips. I make boards with popular TV shows, movie clips, and musical artists. This usually sparks their interest and it is fun for me!